MS researchers are considering the ongoing deterioration that occurs in the MS brain, even when patients are treated with current MS medications. This leads to ongoing progression, damage beyond lesions and relapses which may be related to gray matter atrophy. The new term used to describe this underlying process is "smoldering (or smouldering) disease". Literally, smoke, but no flame.
Despite therapeutic suppression of relapses, multiple sclerosis (MS) patients often experience subtle deterioration, which extends beyond the definition of "progression independent of relapsing activity." We propose the concept of smouldering-associated-worsening (SAW), encompassing physical and cognitive symptoms, resulting from smouldering pathological processes, which remain unmet therapeutic targets. We provide a consensus-based framework of possible pathological substrates and manifestations of smouldering MS, and we discuss clinical, radiological, and serum/cerebrospinal fluid biomarkers for potentially monitoring SAW. Finally, we share considerations for optimizing disease surveillance and implications for clinical trials to promote the integration of smouldering MS into routine practice and future research efforts. https://pubmed.ncbi.nlm.nih.gov/39051525/
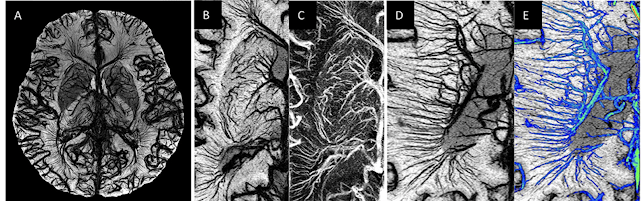
Long time readers of the blog will recognize my questioning this very situation----the ongoing disease progression and loss of grey matter in "treated" MS patients. In 2012, I put together a theory of hypoperfusion and reperfusion injury to address the ongoing, unseen disease progression.
Hypoperfusion/Reperfusion Injury in MS
https://ccsviinms.blogspot.com/2013/09/multiple-sclerosis-hypoperfusionreperfu.html
Even though I am not currently writing for this blog, I do check it occasionally--and have noted that people are still finding it and reading the posts. In fact, over a million readers from all over the globe have read a variety of posts since I began writing. Just today, there were 259 readers, yesterday there were 1223. Over 30,000 unique readers check out the blog posts each month. Obviously, there is still an interest in the vascular connection to MS.
In this new era of AI--I am able to ask the computer/hive mind what it thinks about "smoldering disease" in MS being related to hypoperfusion and hypoxia in the MS brain.
And AI seems to think it might be something worth exploring! Perhaps this theory might be worth investigating.
- Smoldering lesions: These are chronic, active MS lesions characterized by ongoing low-grade inflammation and tissue damage, contributing significantly to disease progression and disability accumulation, even when there are no outward signs of a relapse.
- Hypoperfusion in MS: Research indicates that many individuals with MS experience widespread cerebral hypoperfusion, meaning reduced blood flow to their brain. This hypoperfusion can lead to areas of oxygen deficiency (hypoxia).
- Hypoxia and Inflammation Cycle: Hypoxia and inflammation are closely intertwined in MS. Hypoxia can exacerbate inflammation, while inflammation can trigger hypoxia by damaging blood vessels and impairing blood flow regulation. This creates a vicious cycle that contributes to MS disease progression.
- Smoldering Lesions and Hypoxia: Hypoxia may play a crucial role in the development and persistence of smoldering lesions, particularly pattern III lesions which show similarities to hypoxic/ischemic lesions. Studies suggest that chronic inflammation associated with smoldering lesions, especially those containing iron-laden microglia/macrophages at their edge, could contribute to local tissue hypoxia and chronic damage.